Mouse Model of LEMS Provides New Tool to Develop Therapies
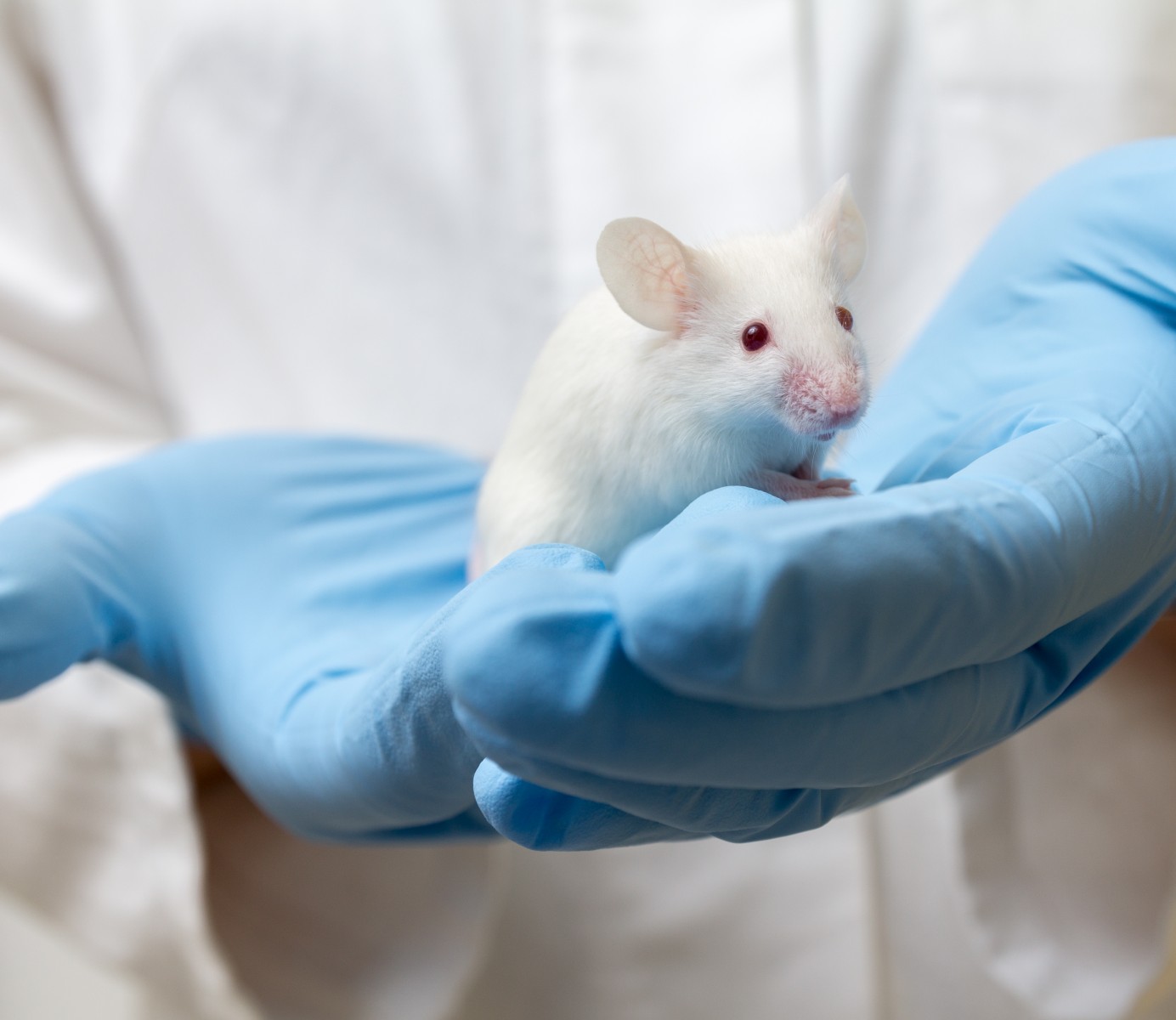
An animal model of Lambert-Eaton myasthenic syndrome (LEMS) has enabled better understanding of what drives the hallmark reduction in acetylcholine release as well as effective testing of treatment candidates.
The study, “Lambert-Eaton myasthenic syndrome: mouse passive-transfer model illuminates disease pathology and facilitates testing therapeutic leads,” appeared in the journal Annals of the New York Academy of Sciences.
LEMS is caused by the production of antibodies targeting voltage-gated calcium channels at the neuromuscular junction — the site where muscles and nerve cells connect — impairing the release of the neurotransmitter acetylcholine. However, characterization of acetylcholine release is needed to better understand disease processes and to design treatment strategies.
Using mice, researchers have found that each neuromuscular junction, or synapse, has about 700 transmitter release sites. Each release site contains an average of two tiny vesicles containing acetylcholine, but only 70–100 of these vesicles are released upon activation, which indicates that each active zone has a low probability of releasing the transmitter.
Approximately half of LEMS patients develop cancer, especially small cell lung cancer. Tumor cells in the lungs have the same types of calcium channels and secretory machinery as nerve terminals. As a result, patients with LEMS may have autoantibodies specific to proteins other than the P/Q-type calcium channels, the most common targets in this disease.
An animal model of LEMS able to accurately reflect disease processes has been developed by injecting patient antibodies into mice, a so-called passive-transfer approach. Twenty-four hours after injecting the antibodies, the mice are given the immunosuppressant cyclophosphamide, followed by new administrations of patient serum or plasma over 14–30 days to generate the disease profile.
Several studies have shown significant reductions in acetylcholine release with this approach, as well as disrupted organization and lower number of active zones, or acetylcholine release sites. This led to the hypothesis that neuromuscular junctions of mice with LEMS have fewer calcium channels, which was supported by marked reductions in calcium currents upon stimulation.
Also, pharmacological studies revealed alterations in the calcium channel subtypes, with a reduced role of P/Q-type channels in acetylcholine release. This is interpreted as a mechanism used by nerve cells to compensate against the attack by autoantibodies, the team from the University of Pittsburgh and the Icahn School of Medicine at Mount Sinai said.
The primary treatment approach in LEMS aims to increase acetylcholine release. It uses a potassium channel blocker such as Firdapse (amifampridine, by Catalyst Pharmaceuticals) with or without a blocker of the enzyme acetylcholinesterase, responsible for the breakdown of acetylcholine. However, side effects such as fatigue and seizures often result in therapy doses not high enough to provide clinical benefits.
Taking advantage of the passive-transfer mouse model of LEMS, scientists have developed a compound known as GV-58, which is an agonist (activator) of calcium channels and is similar to a molecule called (R)-roscovitine. Both GV-58 and (R)-roscovitine selectively target P/Q- and N-type calcium channels, ultimately increasing acetylcholine release.
Scientists have found that GV-58 doubles acetylcholine release from the neuromuscular junction of mice, a similar effect to that of clinically relevant doses of Firdapse. GV-58 holds calcium channels open longer, thereby increasing the likelihood of neurotransmitter release. A combination of GV-58 with Firdapse, which increases the number of open channels, led to more pronounced effects than either compound alone.
Current efforts intend to determine behavioral effects in the passive-transfer model of LEMS. However, the variable results found to date highlight the importance of carefully choosing the patient serum to trigger the disease, the investigators noted.
“In summary, the mouse neuromuscular junction and associated LEMS passive-transfer model have been very effective animal models,” the scientists said. “Furthermore, using the mouse LEMS passive-transfer model, novel therapeutic approaches have been tested effectively.”