Autoantibodies Targeting GRP78 Protein May Cause PCD in LEMS
Written by |
Autoantibodies against a protein called GRP78 may lead to paraneoplastic cerebellar degeneration (PCD) in people with Lambert-Eaton myasthenic syndrome (LEMS), a study suggests.
The study, “GRP78 antibodies are associated with blood-brain barrier breakdown in paraneoplastic cerebellar degeneration in Lambert‐Eaton myasthenic syndrome,” was published in the journal Clinical and Experimental Neuroloimmunology and provided an overview of the team’s work on PCD in LEMS patients.
Autoantibodies are antibodies that wrongly target the body’s own cells. People with LEMS have autoantibodies specific to P/Q-type voltage-gated calcium channels (VGCCs), which impair the communication between motor nerve terminals and muscles and cause muscle weakness.
These channels are also found in Purkinje cells, a type of neuron that is located in the cerebellum, a region of the brain important for coordinating movement.
PCD is characterized by the loss of Purkinje cells. Less than 10% of people with LEMS will also develop PCD, collectively referred to as PCD-LEMS. Even outside the context of LEMS, PCD is often associated with autoantibodies against VGCCs.
From these data, it has been suggested that autoantibodies against P/Q-type VGCCs are a cause of PCD. But why only some people with these autoantibodies develop PCD remains unknown.
The answer may be that anti-VGCC autoantibodies are not always able to get into the brain to attack Purkinje cells because of the blood-brain barrier, which is essentially a membrane that carefully controls which molecules and cells from the blood can or cannot get into the brain.
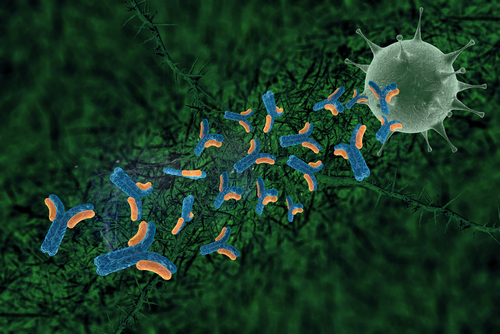
Previous research has shown that autoantibodies isolated from PCD-LEMS patients and specific to the protein GRP78 can bind to cells in the blood-brain barrier, as assessed in a model created in the lab. This binding increased the membrane’s permeability by lowering the levels of a protein called claudin-5.
As such, antibodies against GRP78 may weaken the integrity of the blood-brain barrier by allowing anti-VGCC autoantibodies to get into the brain and cause PCD. From this model, it would be expected that people with PCD-LEMS would have anti-GRP78 autoantibodies, in contrast to patients with LEMS but not PCD.
In fact, 15 of 18 (83.3%) patients with PCD-LEMS had antibodies against GRP78, with only one of the 15 patients (6.6%) with LEMS but not PCD showing such autoantibodies in the blood. None of the eight controls had detectable GRP78 autoantibodies.
Additionally, removing the GRP78 autoantibodies from the samples tested in the blood-brain barrier model lessened the effect on the membrane’s permeability.
“These findings indicate that GRP78 autoantibodies from PCD-LEMS patients allowed the entry of [disease-causing] P/Q-type VGCC autoantibodies into the CNS [central nervous system] via [blood-brain barrier] dysfunction,” the researchers wrote.
They further said that GRP78 is expressed by several types of cancer cells, which could suggest that GRP78 autoantibodies could be a product of the body’s immune response against a tumor.
The same process is also how most cases of LEMS are caused: Cancer cells — particularly small cell lung cancer cells — express P/Q-type VGCCs, and autoantibodies are produced as a result of the immune response against the tumor.
“We concluded that GRP78 autoantibodies are produced by an autoimmune response against cancer and might act in concert with P/Q type-VGCC antibodies through [blood-brain barrier] breakdown to cause CNS symptoms in patients with PCD-LEMS,” they said.