Firdapse (amifampridine) for Lambert-Eaton myasthenic syndrome
Last updated Oct. 1, 2024, by Marisa Wexler, MS

What is Firdapse for Lambert-Eaton myasthenic syndrome?
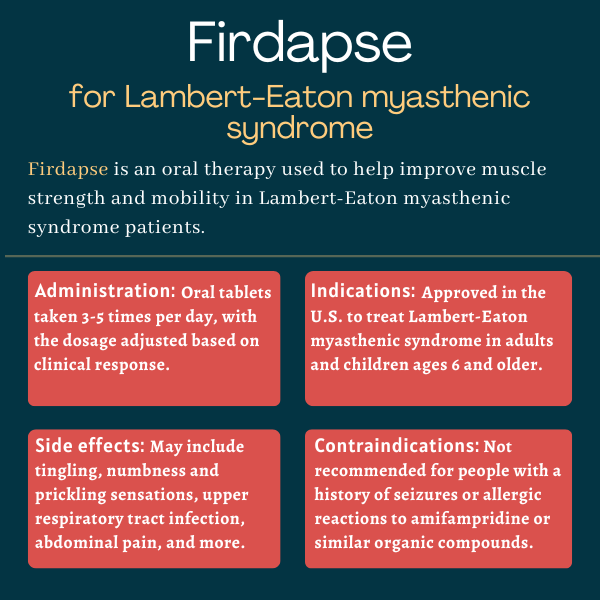
Firdapse (amifampridine) is an oral therapy for the symptomatic treatment of Lambert-Eaton myasthenic syndrome (LEMS). It works to improve muscle strength and mobility in adults and children with the autoimmune disease.
It is the only orally available treatment approved in the U.S. for LEMS symptoms.
The medication was originally developed by BioMarin Pharmaceutical, but its licensing rights in North America have belonged to Catalyst Pharmaceuticals since October 2012. In subsequent agreements, Catalyst has expanded its rights to develop and market Firdapse in other markets, including parts of Asia and South America. In Japan, Firdapse is being developed by the company in partnership with DyDo Pharma.
Therapy snapshot
| Brand name: | Firdapse |
| Chemical name: | Amifampridine |
| Usage: | Symptomatic treatment of Lambert-Eaton myasthenic syndrome |
| Administration: | Oral tablets taken by mouth 3-5 times daily |
How does Firdapse work?
LEMS develops because the body makes self-reactive antibodies, called autoantibodies, against a protein known as voltage-gated calcium channel or VGCC, which is found on nerve cell endings. As a result, nerve cells are prevented from taking up calcium, which is required for the release of a neurotransmitter, or cell-signaling molecule, called acetylcholine.
Acetylcholine is normally released into the neuromuscular junction — the point where nerve and muscle cells come into contact — to trigger muscle contraction. In patients with LEMS, however, little acetylcholine is released, resulting in muscle weakness and fatigue.
Firdapse is a small molecule that nonspecifically blocks another protein channel, called voltage-dependent potassium channel, found on nerve cells, effectively preventing potassium ions from leaving nerve cells. This causes any remaining healthy VGCCs to stay open, allowing for the influx of calcium ions into nerve cells. That potentially increases the amount of acetylcholine released from nerve cell endings, which in turn is expected to help enhance muscle strength.
Who can take Firdapse?
Firdapse is the first and only oral therapy available in the U.S. for the symptomatic treatment of LEMS. The U.S. Food and Drug Administration (FDA) approved the therapy in November 2018 for patients ages 17 and older.
That approval was expanded in October 2022 to include children as young as 6. The decision followed the cancelation of the regulatory approval of Ruzurgi, a therapy containing the same active ingredient as Firdapse. In the U.S., Ruzurgi had previously been approved to treat children and adolescents with LEMS.
In the European Union, Firdapse was approved by the European Commission in 2009 for commercial use. In 2020, Canada’s regulatory agency approved the use of Firdapse for the treatment of adults with LEMS. Japan’s regulatory health agency approved Firdapse for the treatment of LEMS in 2024.
Who should not take Firdapse?
Firdapse is contraindicated, or not recommended, for people with a history of seizures and allergic reactions to amifampridine or similar organic compounds. The medication should be stopped if seizures or life-threatening allergic reactions occur.
The safety and effectiveness of Firdapse for the treatment of LEMS in children younger than 6 have not been established.
How is Firdapse administered?
The therapy is available as oral tablets containing 10 mg of amifampridine. Tablets have a white to off-white color and a round shape, and are functionally scored to facilitate splitting into fractions. Treatment is supplied both in bottles and blister packs that should be stored at room temperature.
The recommended starting dose for adults and children weighing 45 kg (99 pounds) or more is 15 to 30 mg daily, taken in 3-5 divided doses, with no more than 20 mg taken at any one time. If needed, the medication’s total daily dosage can be increased by 5 mg daily every three to four days. The maximum recommended dose is 100 mg per day.
For children weighing less than 45 kg, the recommended starting dose is 5 to 15 mg daily, also taken in 3-5 divided doses, with each dose not exceeding 10 mg. Firdapse’s total daily dosage also can be increased for these patients, by 2.5 mg daily every three to four days, if needed. The maximum recommended total daily dose in these patients is 50 mg per day.
In patients with kidney or liver impairments, or for those who are known to process the medication’s active ingredient at a slower pace, the recommended starting dose should be the lowest initial recommended daily dosage in each group — 15 mg daily for adults and children weighing 45 kg or more, and 5 mg daily for pediatric patients weighing less than 45 kg.
The medication can be taken with or without food. If a dose is missed, patients should not take a double dose or additional doses to compensate for the missed one.
In patients requiring small dosage increments (less than 5 mg), or in those having difficulty swallowing tablets or requiring a feeding tube, Firdapse can be administered in a 1 mg/mL liquid suspension. The suspension can be prepared by placing the required number of tablets in a 50 to 100 mL container and adding 10 mL of sterile water for each tablet, then waiting for five minutes. Once prepared, the suspension can be given to patients by mouth with the help of an oral syringe, or via a feeding tube.
Firdapse in clinical trials
Firdapse’s approval was based on positive results from two Phase 3 randomized, double-blind, placebo-controlled trials. In these trials, dubbed LMS-002 and LMS-003, neither the researchers nor the participants knew which patients were receiving Firdapse and which were given the placebo. All patients in both studies were on a stable dose of Firdapse prior to being randomly assigned to either continue treatment with the therapy or be given the placebo.
LMS-002 trial
LMS-002 (NCT01377922) involved 38 LEMS patients who were initially assigned to either continue treatment with Firdapse or to receive a placebo for seven days. After this initial period, patients remained on Firdapse or the placebo for a second seven-day period.
Changes from baseline, or the study’s start, were analyzed at day 14 for both the Firdapse and the placebo treatment groups. Several measures, including quantitative myasthenia gravis, or QMG, and subject global impression, or SGI, scores, were evaluated for changes. QMG is a 13-item scale a physician uses to grade a patient’s muscle weakness. The SGI score is a seven-point scale in which patients rate the global impression of the effects of the study treatment on their overall well-being.
Other measures included the clinical global impression-improvement (CGI-I), a seven-point scale used by physicians to grade changes in patient symptoms, behavior, and functional abilities.
QMG and SGI scores tended to worsen in both groups. However, in patients given the placebo, the degree of worsening was significantly greater than that seen among those treated with Firdapse. Additionally, CGI-I scores were significantly higher in patients given the placebo, indicating that physicians perceived greater disease worsening in that group of patients compared with those treated with Firdapse.
LMS-003 trial
LMS-003 (NCT02970162) involved 26 adults with LEMS and analyzed the efficacy of Firdapse over a four-day period. The participants were on a stable dose of Firdapse for at least one week before the study. After baseline measurements on day 0, patients were randomly assigned to either continue treatment with Firdapse or to receive a placebo from day 1 to day 3. They then were assessed after taking their medication on day 4.
The results showed significant benefits of Firdapse over the placebo in all parameters analyzed, including CGI-I, QMG, and SGI scores. Mild adverse events or side effects, such as back pain, pain in the extremities, or headaches, were noted in those being treated with Firdapse, whereas those given a placebo reported fatigue and muscle weakness, which was expected due to Firdapse withdrawal.
Common side effects of Firdapse
The most common side effects associated with Firdapse include:
- tingling, numbness, or prickling in the skin, known as paresthesia
- upper respiratory tract infection
- abdominal pain
- nausea
- diarrhea
- headache
- liver dysfunction
- back pain
- high blood pressure
- muscle spasms.
Seizures
Patients may experience seizures while on Firdapse — and these may occur in individuals without a history of such episodes. If there are seizures, patients are recommended to stop taking the medication or reduce its dosage.
Allergic reactions
Firdapse itself has not been reported to cause allergic reactions in trials. But similar compounds have been known to sometimes cause allergic reactions, including anaphylaxis, which can be serious and life-threatening. If anaphylaxis occurs, the medication should be stopped and appropriate treatment administered.
Use with other medications
People who take Firdapse alongside medicines used to treat seizures are more likely to experience seizures. The therapy’s simultaneous use with cholinesterase inhibitors — a group of medicines that block the normal breakdown of acetylcholine — may increase the cholinergic effects of Firdapse and of those medicines, and heighten the risk of side effects.
Use in pregnancy and breastfeeding
According to animal data, Firdapse may cause harm to a developing fetus. Therefore, patients who are pregnant or are planning to become pregnant should discuss this issue with their healthcare team. All patients breastfeeding or planning to breastfeed should also inform their healthcare provider, as it is not clear if Firdapse can pass into breast milk, or be harmful to the nursing infant.
Patients who have been exposed to Firdapse while pregnant may enroll in the Firdapse Pregnancy Registry, which was created to monitor pregnancy and newborn outcomes.
Lambert-Eaton News is strictly a news and information website about the disease. It does not provide medical advice, diagnosis, or treatment. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.
Recent Posts
- Facing long-distance travel challenges after a LEMS diagnosis November 11, 2024
- NORD offering financial support program to cover LEMS costs November 5, 2024
- The challenges of maintaining a healthy weight with LEMS October 28, 2024
- Coping with loss, big and small, in the wake of a LEMS diagnosis October 14, 2024
- Firdapse approved to treat LEMS patients in Japan October 1, 2024
- A friend with LEMS shares her pregnancy journey September 30, 2024
- The LEMS community is making progress through advocacy September 23, 2024
- Oh, for a place where everybody knows your name September 9, 2024
- Firdapse is effective in LEMS, even with delay in starting treatment September 3, 2024
- A friend’s journey with Lambert-Eaton myasthenic syndrome August 26, 2024
Related articles



