Weighing the Pros and Cons of My Daughter’s IVIG Therapy
Written by |

The first question I asked after my daughter Grace was diagnosed with Lambert-Eaton myasthenic syndrome (LEMS) was what types of treatments were available to her. I do not take it for granted that treatment is available, because I know many other rare diseases do not afford the same opportunity.
Before she had been diagnosed, Grace’s neurologist started her on Mestinon (pyridostigmine), originally thinking Grace might have myasthenia gravis. This was her first line of treatment, and it helped a bit with symptoms such as slurring words and swallowing, but had little impact on her ability to walk.
Once she had a confirmed diagnosis, Grace’s neurologist suggested she begin taking Ruzurgi (amifampridine), which had just become the first treatment approved by the U.S. Food and Drug Administration specifically for children with LEMS. She started on a very low dose, as is protocol, and we saw gradual improvement as her dosage increased.
Because my daughter’s LEMS had been triggered by an autoimmune response, rather than a cancer diagnosis, many of the available treatments focus on manipulating her immune system.
After three months on Ruzurgi, Grace was still very unsteady on her feet and was unable to get out of bed on her own in the morning. Grace’s neurologist suggested she begin intravenous immunoglobulin (IVIG) therapy, which is manufactured from donated healthy plasma.
Thankfully, the LEMS community helped prepare us for that first treatment. They told us that one of the most important things to do before IVIG treatment is to hydrate, hydrate, hydrate. We started pushing the fluids in hopes of staving off the common side effect of headache, along with preparing Grace’s vein for an IV.
Usually, IVIG is administered every three to four weeks over a period of several hours or days, depending on the patient’s needs.
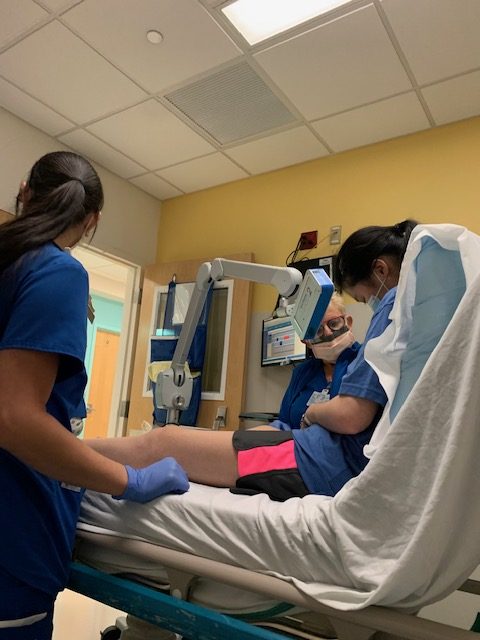
Grace receives her IVIG treatment at our local children’s hospital as an outpatient in their day hospital. The medical staff begins by giving her Benadryl and Tylenol to preempt any allergic reactions.
The first round of IVIG took about seven hours. The drip ran very slowly, and she finished with a saline drip.
The morning after her first IVIG treatment, Grace woke with a massive headache and felt unusually sluggish until her morning medicine kicked in, which took much longer than normal. Approximately four days after her first treatment, Grace began to feel an uptick in her energy and strength.
Over the course of the year since Grace started IVIG, we have had to weigh the good against the bad as we determine if this is the best course of treatment for her. IVIG gives her a much-needed boost of energy for about three weeks. Grace claims it helps with her sleep (falling asleep and staying asleep), along with increased stability on her feet.
One of the drawbacks of IVIG is definitely the time it takes out of her schooling and schedule to accommodate the two days a month spent at the hospital. Going forward, we will have to weigh this as she begins college and a career.
Along with the time commitment, another drawback is the wear and tear on her veins. It has gotten increasingly hard for the nurses to find a good vein to access for treatment. Many patients decide a port is the easiest solution, but for now we hold off on that decision.
With each new treatment, I found I had to temper my expectations. Usually, I went into the new treatment feeling very hopeful about a massive change in her mobility and symptoms. Many people within the LEMS community experience differing levels of effectiveness from the treatments available.
After reading the best-case scenarios, I dealt with a lot of disappointment when Grace did not achieve those same results. Each of the treatments help in varying ways, but none of them have been the “overnight” change I wanted and hoped for.
I found it most helpful to manage my expectations and cement in my mind that we are running a marathon, not a sprint. We may not see the spectacular change other patients do with various treatments and medicines, but we are grateful for the slow increase in her abilities as we add to and tweak her treatment plan.
I am truly grateful that she even has a treatment plan.
***
Note: Lambert-Eaton News is strictly a news and information website about the disease. It does not provide medical advice, diagnosis, or treatment. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website. The opinions expressed in this column are not those of Lambert-Eaton News or its parent company, Bionews, and are intended to spark discussion about issues pertaining to Lambert-Eaton myasthenia.





Joyce Crawford
Lori, I just read your post while getting my second dose of IVIG. I have been researching about this treatment and found many references to getting the IG by subq infusions either as outpatient or at home. There are many advantages to the subq, one of which is not needing to have vein access. Maybe Grace would do better with this method. The blood levels of IG are much more steady also with the subq. There are several options of dosing with the subq. Hopefully her doctor could check on it for her. Good luck, Joyce Crawford
Lori Dunham
Hi Joyce. Yes, I have also heard about the subq option and will definitely keep it in mind for Grace. I plan to talk to her doctor about it. I really think it's beneficial for not needing vein access and I love the idea that she wouldn't necessarily have the ups and downs she does with ivig. I hope your treatment goes well and I thank you for this information. It's definitely an option people need to know about.