Study Reports Rare Case of Non-small Cell Lung Cancer in Patient with LEMS and Paraneoplastic Cerebellar Degeneration
shutterstock/Von solar22
A rare case of non-small cell lung cancer (NSCLC) was discovered in a patient with paraneoplastic cerebellar degeneration and Lambert-Eaton myasthenic syndrome (PCD-LEMS) — the first report to link the cancer to late-onset PCD-LEMS, according to researchers.
Their study, “Non-small cell lung cancer associated with late-onset Lambert–Eaton myasthenic syndrome and paraneoplastic cerebellar degeneration” was published in the journal Neurological Sciences.
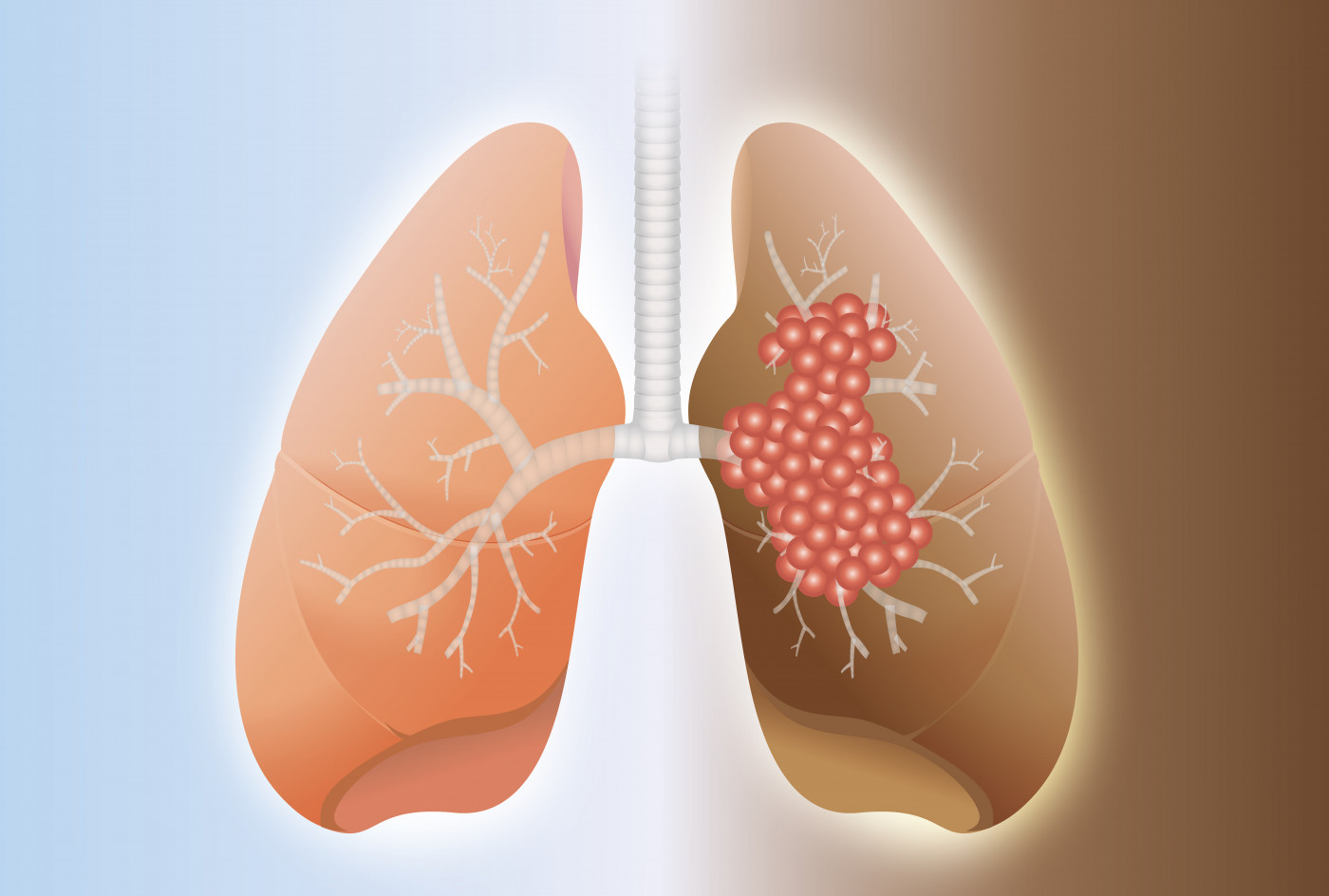
The majority of patients with PCD-LEMS have an underlying tumor, the most common being small cell lung cancer, one of the two main forms of lung cancer. The other type is non-small cell lung cancer (NSCLC).
In this case study, a team of researchers in China reported for the first time a case of NSCLC in a patient with late-onset PCD-LEMS.
The 65-year-old woman was admitted to the hospital after experiencing cough, expectoration (coughing up phlegm or mucus), and hemoptysis (coughing up of blood) for two months. A computed tomography scan revealed the existence of tumors in both lungs and enlargement of the lymph nodes in the mediastinum (the region located in the chest between the sternum and the spinal column).
Positron emission tomography (PET) scan also indicated the presence of tumors in the lungs and mediastinum. PET imaging uses small amounts of radioactive materials, called radiotracers, along with a special camera and computer, to help evaluate organ and tissue function and aid diagnosis.
After a biopsy of the lungs, the patient was diagnosed with late-stage NSCLC and began treatment with chemotherapy. She was given six cycles of a chemotherapy combo, pemetrexed and cisplatin, delivered intravenously (into the blood).
However, the patient experienced only partial response. She received four cycles of maintenance chemotherapy with pemetrexed alone, leading to stabilization of the cancer. After four cycles of maintenance chemotherapy, there were no signs of cancer recurrence.
After four months, the patient began to feel tired, with sudden dizziness and mild nausea but without headache or a need to vomit. Within three weeks, the patient developed speech problems (dysarthria), unsteady gait, and muscle fatigue while walking, as well as ataxia. Other symptoms included dry mouth and constipation.
She was admitted to the hospital again, and physical examination revealed no signs of tumor metastasis in the brain. Moreover, there were no significant changes in the tumor’s mass in the lungs, and no enlarged lymph nodes.
Blood test analysis showed elevated levels of antibodies against the body’s own voltage-gated calcium channels of the P/Q-type, a group of ion channels on the surface of cells, and antineuronal antibodies, specifically anti-Yo.
Anti-Yo antibodies target Purkinje neurons, which are nerve cells located in the brain region called the cerebellum. Moreover, anti-Yo antibodies have been associated with PCD.
The patient was diagnosed with PCD-LEMS “11 months after diagnosis of NSCLC and 5 weeks after the onset of neurological dysfunction,” the researchers wrote.
The patient began treatment with Firdapse (amifampridine, also called 3,4‐diaminopyridine or 3,4‐DAP), an approved LEMS treatment. The treatment led to a significant lessening of muscle weakness, dry mouth, and constipation.
Additionally, the patient was treated with a large dose of a corticosteroid to suppress the immune system called Medrol (methylprednisolone) and intravenous immunoglobulin for one week, which reduced her neurological symptoms.
After 10 weeks, she showed no signs of weakness, dry mouth, constipation, or diplopia (double vision). She remained with difficult or unclear articulation of speech (dysarthria) and impaired coordination and balance, but was able to walk without assistance.
“The patient was still alive for 19 months, and the recent examination was still without signs of recurrence of neurological symptoms and tumors,” the researchers stated. “To the best of our knowledge, this was the first case report describing that PCD-LEMS existed in a patient with NSCLC.”
Interestingly, they also discovered that “patients with PCD-LEMS seemed to have a better neurological improvement through anti-tumor treatment or immunotherapy compared to those with PCD only, indicating that LEMS may have an effect on the immune response of PCD and the specific mechanism [should] be further explored.”






